According to the Global Cancer Observatory by the World Health Organization International Agency for Research on Cancer, breast cancer was the most common cancer in the Philippines in 2022. It also claimed close to 12,000 lives in the Philippines that year, making it the country’s second leading cause of cancer-related deaths after lung cancer.
On May 26, an article by Harvey Sapigao reported that UP biologists have developed a model capable of detecting lymphovascular invasion (LVI). LVI occurs when cancer cells invade the lymphatic and blood vessels, allowing the cancer cells to spread to various parts of the body. The LVI serves as an early indicator of metastasis, and presently, can only be “detected by examining tissue surrounding the tumor that has been surgically removed,” Sapigao noted.
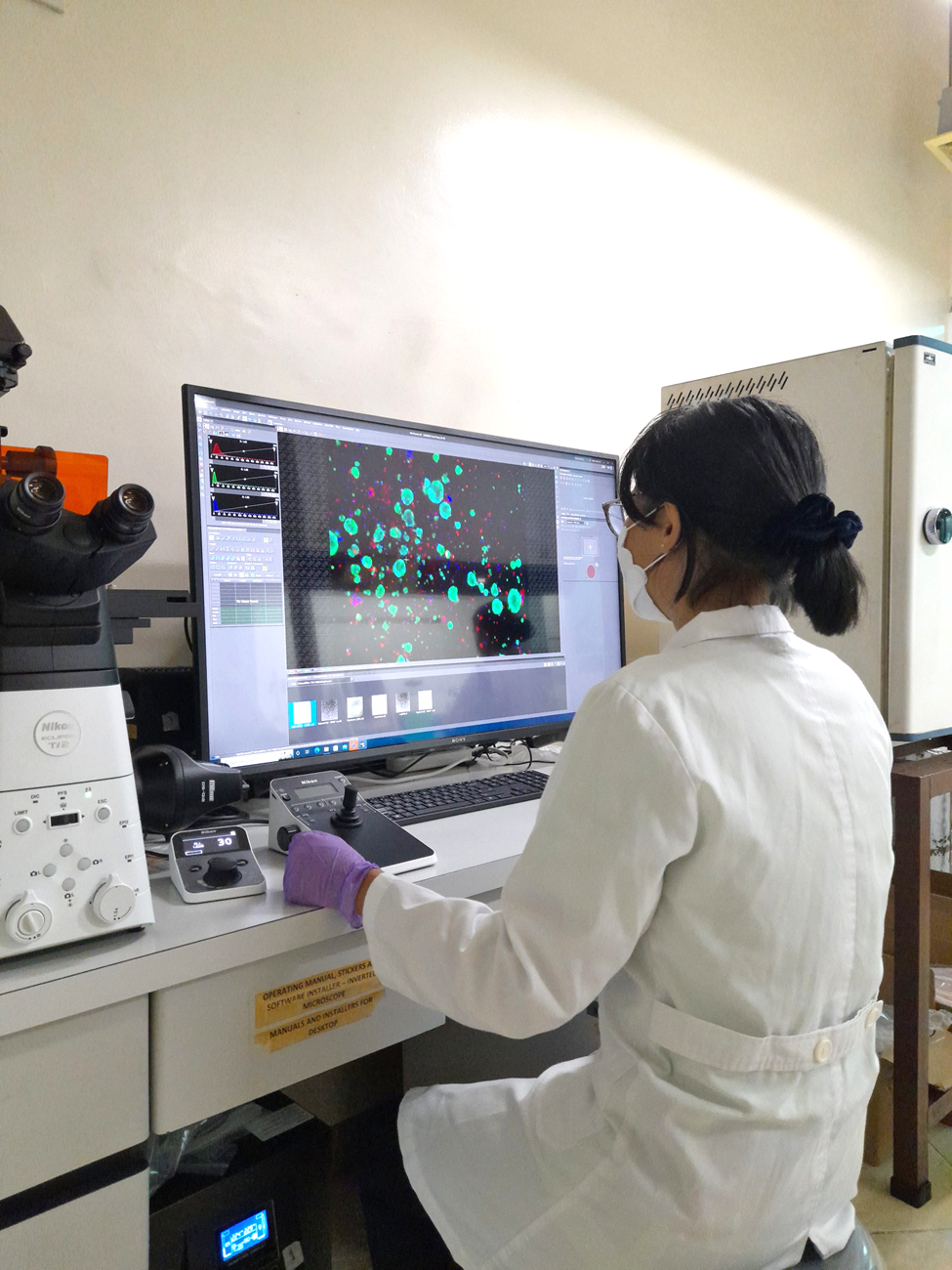
Sapigao, in his article UP-developed Model Shows Promise in Detecting Early Signs of Metastasis in Breast Cancer Patients, stated that the UP biologists developed a mathematical model “that can detect LVI in breast cancer patients even before surgical treatment. Their study also revealed links between LVI and drug resistance, helping explain why breast cancer patients with LVI respond poorly to anticancer drugs.”
Michael C. Velarde, PhD, professor at the UP Diliman Institute of Biology (IB), emphasized the significance of early detection: “If we can detect LVI earlier, doctors could personalize patient treatment and improve their outcomes. This could help avoid ineffective treatments and focus on strategies that work better for aggressive breast cancer.”
Velarde is the study’s author, along with Allen Joy M. Corachea and Regina Joyce E. Ferrer, science research specialists at the IB; Lance Patrick Ty and Madeleine T. Morta, researchers at the IB; and researchers from the Philippine Genome Center and UP Manila.
The researchers found that patients with LVI are abundant with UGT1 and CYP genes, genes involved in breaking down anticancer drugs. These genes accelerate drug breakdown, reducing treatment effectiveness. The article also states that patients with more UGT1 and CYP genes “are more likely to have tumors that survive chemotherapy and eventually metastasize.”
Sapigao’s article detailed that the team “developed a regression model that analyzed the expression patterns of UGT1 and CYP genes” and that the model “correctly predicted LVI status at the time of biopsy and before surgery 92% of the time.”
Although the model is still in its early development and more validation studies are still needed, once these are addressed, Velarde in the article noted that the approach “can be implemented in the Philippines using locally available genomic technologies, making earlier detection and tailored treatment more accessible to Filipino patients.”
The authors also plan to further investigate “how UGT1 and CYP genes are related to LVI to identify drug combinations that work better for LVI-positive patients” so as to “develop a practical test that can be used in Philippine hospitals to guide doctors in choosing the best treatment for each patient,” the article states.—With a report from the UP Diliman College of Science